By: Dr. Shaum Bhagat
 The risk of suffering a fall causing significant injury, such as a broken hip, increases exponentially with age. Many elders are interested in learning about improving their balance and equilibrium in their daily living to prevent falls from occurring. In some cases, disturbances in balance and equilibrium can be attributed to age-related changes in the inner ear. Each ear can be categorized into three main components: the outer ear, the middle ear, and the inner ear. The inner ear is a tiny fluid-filled structure housed deep within the temporal bone of the skull. The inner ear contains five sensory organs contributing to balance and equilibrium and one sensory organ for hearing. The sensory organs for balance and equilibrium in a given inner ear include the saccule, the utricle, and three semicircular canals. These sensory organs connect to the muscles of the eyes controlling eye movements through complex neural pathways within the brain. Coordinated activity between these inner ear organs and the muscles controlling eye movements contribute to maintaining one’s balance and upright stance.
The risk of suffering a fall causing significant injury, such as a broken hip, increases exponentially with age. Many elders are interested in learning about improving their balance and equilibrium in their daily living to prevent falls from occurring. In some cases, disturbances in balance and equilibrium can be attributed to age-related changes in the inner ear. Each ear can be categorized into three main components: the outer ear, the middle ear, and the inner ear. The inner ear is a tiny fluid-filled structure housed deep within the temporal bone of the skull. The inner ear contains five sensory organs contributing to balance and equilibrium and one sensory organ for hearing. The sensory organs for balance and equilibrium in a given inner ear include the saccule, the utricle, and three semicircular canals. These sensory organs connect to the muscles of the eyes controlling eye movements through complex neural pathways within the brain. Coordinated activity between these inner ear organs and the muscles controlling eye movements contribute to maintaining one’s balance and upright stance.
In elders, the aging process can lead to deterioration of the inner ear sensory organs contributing to balance and equilibrium. In turn, this can lead to the loss of maintenance of balance and an increased risk of falling. Identifying the factors that make elders more susceptible to falls remains an area of intensive research focus.
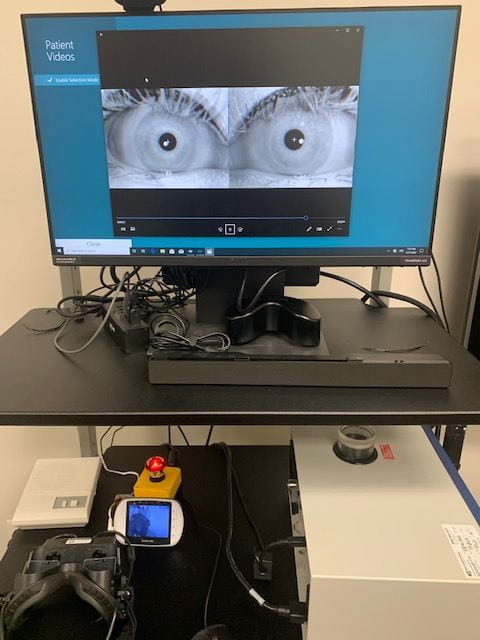 The Vestibular Laboratory in the Department of Audiology is equipped with state-of-the-art instrumentation designed to assess equilibrium and balance. This instrumentation includes videonystagmography goggles with high definition cameras that capture and record eye movements [Insert Photo 1]. The recorded eye movements can be analyzed by Doctor of Audiology students and research faculty members in order to determine if an elderly individual may have an increased risk of suffering a fall. The Vestibular Laboratory is also equipped with a rotary chair system that uses cutting-edge technology [Insert Photo 2]. The rotary chair system provides computerized control of a rotating chair to determine if diminished eye movements associated with age-related compromise of inner ear function occurs while the individual is seated in the rotating chair.
The Vestibular Laboratory in the Department of Audiology is equipped with state-of-the-art instrumentation designed to assess equilibrium and balance. This instrumentation includes videonystagmography goggles with high definition cameras that capture and record eye movements [Insert Photo 1]. The recorded eye movements can be analyzed by Doctor of Audiology students and research faculty members in order to determine if an elderly individual may have an increased risk of suffering a fall. The Vestibular Laboratory is also equipped with a rotary chair system that uses cutting-edge technology [Insert Photo 2]. The rotary chair system provides computerized control of a rotating chair to determine if diminished eye movements associated with age-related compromise of inner ear function occurs while the individual is seated in the rotating chair.
For more information about the Vestibular Laboratory, contact the Department of Audiology at 408-924-1754 or audiology@sjsu.edu.



